Reproductive Surgery
Some women may have difficulty conceiving due to issues related to congenital malformation of the reproductive system or gynecological disease acquired later in life. These may range from a congenital malformation of the uterus or absence of a vagina, to acquired abnormalities such as polyps, fibroids or endometriosis. If such a condition is found during your comprehensive fertility evaluation, it may be necessary to have surgery to correct the problem. Keep reading to learn more about some of the surgical procedures available to our patients.
Hysteroscopy
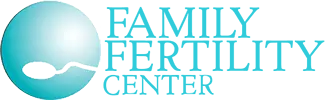
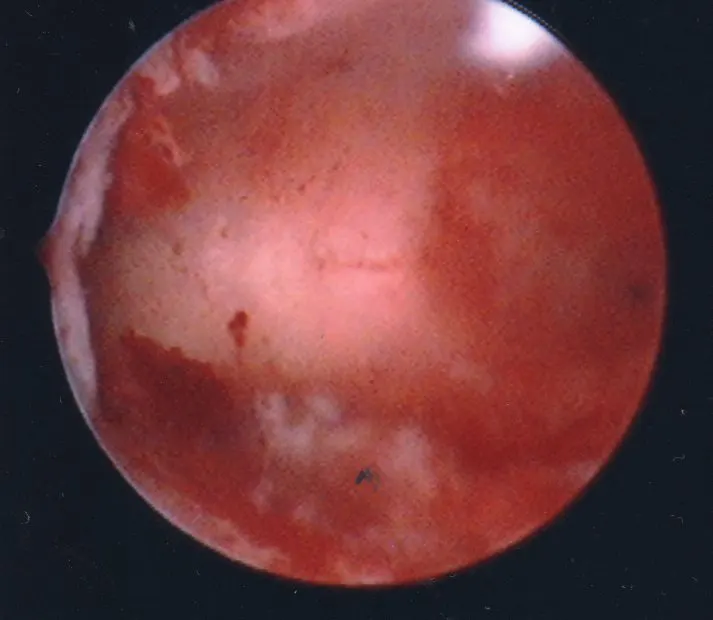
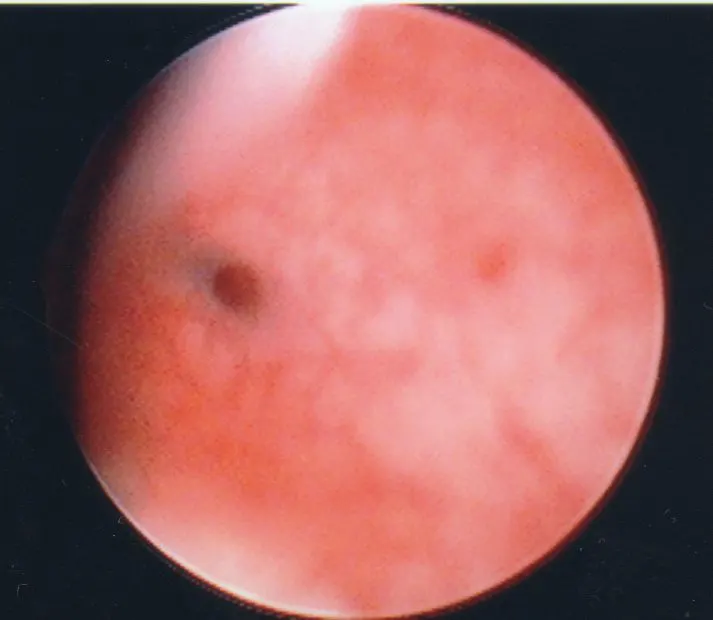
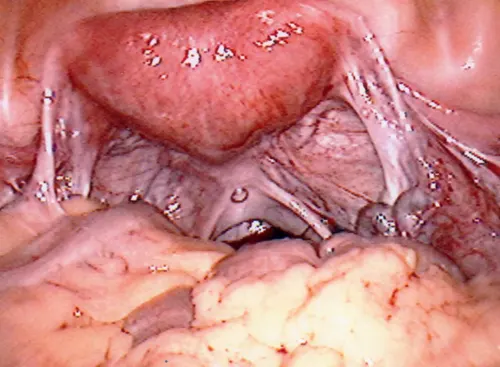
Hysteroscopy is a procedure in which a small, telescope-like instrument is inserted directly into the uterine cavity. The scope allows the surgeon to visualize the uterine cavity and diagnose conditions such as uterine septum (a wall partitioning the uterine cavity partially or completely), scar tissue, uterine polyps, or uterine fibroids. Generally, the anatomical problem can be corrected via the hysteroscope in the same procedure. Hysteroscopy is usually an outpatient surgery which does not require an overnight stay.
First to Last: Hysteroscopic view of a normal uterine cavity; Opening from the corner of the uterus into the fallopian tubes; Polyp inside the uterine cavity; Uterine fibroid within the uterine cavity
Laparoscopy
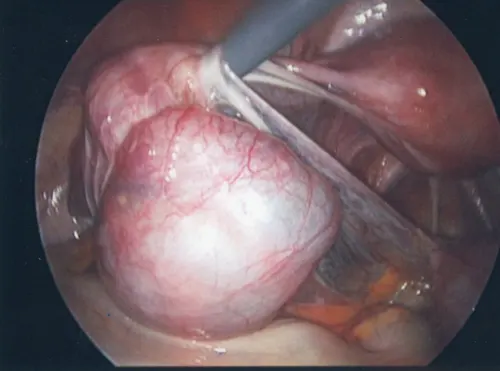
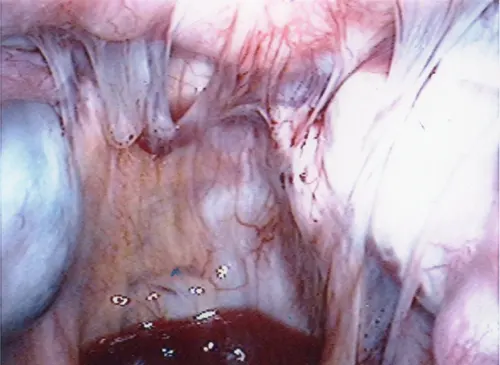
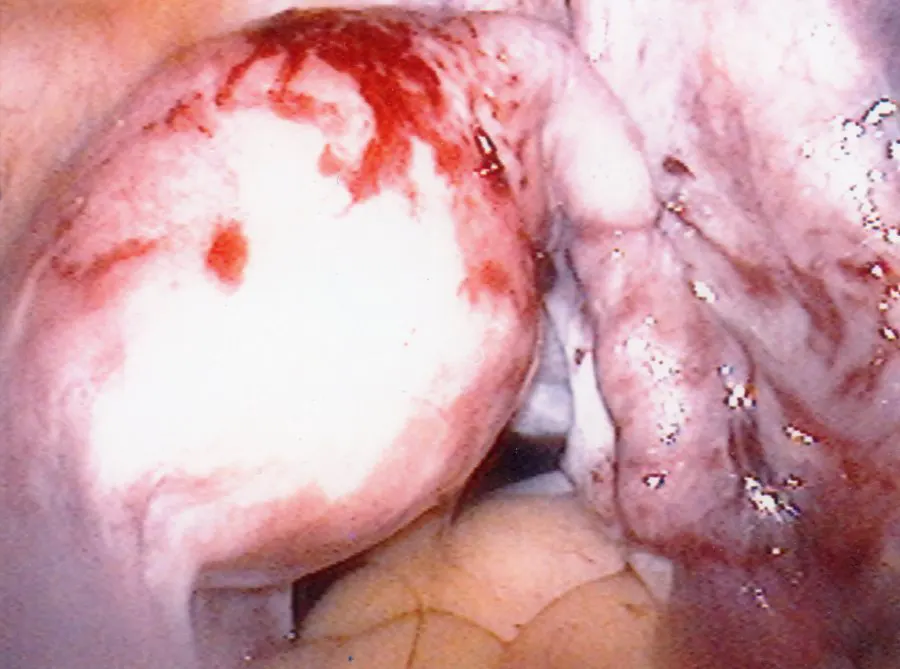
Laparoscopy is a minimally invasive procedure which allows visualization of the pelvic organs. This is performed in an operating room setting where a small telescope-like instrument is inserted through the belly button. With additional small instruments placed strategically through the abdominal wall, the surgeon is able to view and assess the pelvic anatomy. Some of the findings can include endometriosis, tubal damage – (hydrosalpinx – fluid-filled tube), scar tissue, uterine fibroids, ovarian cysts and tumors. Again, the anatomic problem usually can be corrected via the laparoscope in the same procedure. Laparoscopy is an outpatient procedure and often allows the surgeon to correct the pelvic pathology at the same time it is being assessed.
Click here to view a video of diagnostic laparoscopy.
First to Last: Normal ovary and fallopian tubes; Panoramic view of a normal female pelvis; Occluded and dilated fallopian tube (Hydrosalpinx); Pelvic adhesions
Laparotomy
Laparotomy is a procedure in which an abdominal incision is made so as to gain access into the abdominal and pelvic cavities. Typically, this procedure requires a longer recovery time than a laparoscopy because the larger abdominal incision takes longer to heal. In an attempt to expedite recovery from an operation, sometimes a mini-laparotomy may be performed. In a mini-laparotomy, a much smaller incision, 2 to 3 inches as opposed to 4 to 6 inches in traditional laparotomy, is made in the abdominal wall, allowing the patient to go home after a short stay in the hospital. Whether a traditional laparotomy or mini-laparotomy is appropriate depends on the nature and acuteness of pelvic disease. Laparotomy gives the surgeon an opportunity to deal with larger sized pelvic pathology such as uterine fibroids, extremely large ovarian cysts, or a ruptured ectopic pregnancy with uncontrolled hemorrhage. Directly accessing the pelvic area allows the surgeon to address most of the very complex issues that may arise.
Tubal Reversal Surgery
For certain patients who have undergone tubal ligation, a tubal reversal surgery can be performed to reestablish the reproductive communication between sperm and egg. For over 20 years, Dr. H. Christina Lee has performed tubal reversal using micro-surgical techniques via a mini-laparotomy on an outpatient basis. The technique involves making an incision about 2 to 3 inches in width in the abdomen. Using microscopic magnification, meticulous surgical skills and sutures thinner than a strand of human hair, the tubes are reconnected.
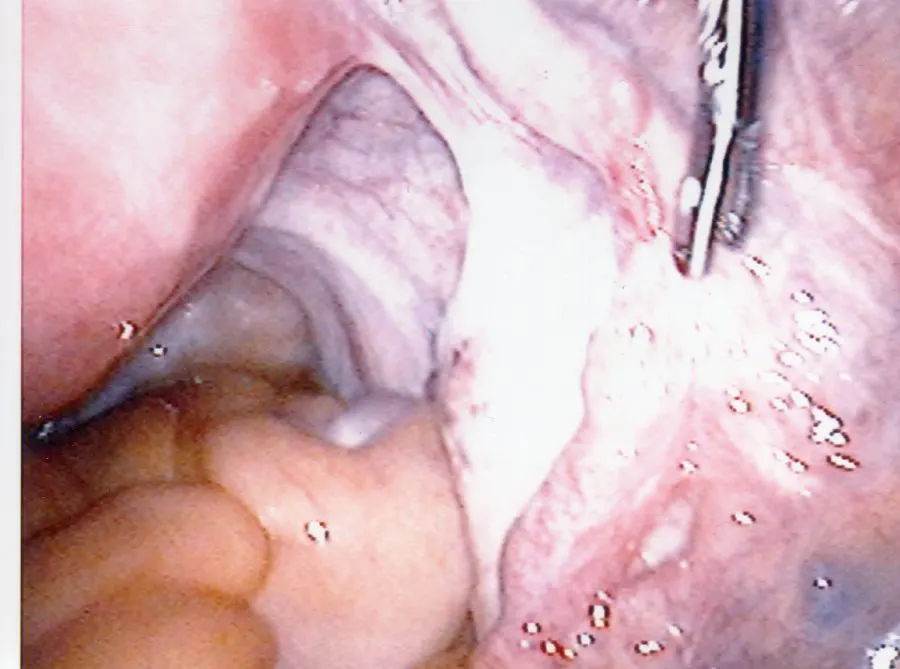
Laparoscopic Tubal Reversal
Recent advances in fiber optic technology provide greater optical magnification and better visualization of details via an operating telescope, called a laparoscope. This technological breakthrough allows the performance of tubal reversal with a laparoscopic approach, obviating the need to make any incision larger than half an inch on the abdominal wall. In a laparoscopic tubal reversal, three or four small incisions, less than half of an inch each, are made on the abdominal wall. Just like the mini-laparotomy approach, the cut fallopian tubes are reattached with fine sutures. The laparoscopic approach is recognized as a minimally invasive procedure, producing less pain after surgery and enabling a much quicker recovery than the traditional open technique. Patient goes home the same day after laparoscopic tubal reversal surgery and returns to work within two to three days.
Top to Bottom: A fallopian tube with missing segment from tubal ligation; Same tube reconnected after laproscopic tubal reversal
Candidate for Tubal Reversal
There are many factors that influence the outcome and determine the appropriateness of this surgery. For instance, a tubal ligation that involves fulguration, or “burning” of the fallopian tubes, is not as easily reversed when compared to a tubal ligation in which a clip has been placed on the fallopian tube.
Prior to surgery, a detailed analysis of the type of tubal ligation previously performed, the likelihood of surgical success, and the best course of action is determined and discussed with the individual or couple. Patients and their partners should complete an infertility evaluation prior to surgery to assure no other infertility factors would compromise outcome. For example, a semen analysis may unveil a previously unknown severe low sperm count in a male partner. Ovarian reserve declines with a woman’s age. Decreased ovarian reserve is associated with lower probability of a live birth. An ovarian reserve evaluation should be done on the female partner to ensure the likelihood of success after tubal reversal surgery.
Schedule a Consultation
Contact Us
If you are experiencing a medical emergency, call 911 or go to the nearest emergency room.
We understand you may have a lot of questions. Additionally, each couple or individual has a unique set of circumstances. To this end, the best way to get answers for your situation is a face-to-face consultation with our physician.
Schedule a Consultation
Contact Us
If you are experiencing a medical emergency, call 911 or go to the nearest emergency room.
We understand you may have a lot of questions. Additionally, each couple or individual has a unique set of circumstances. To this end, the best way to get answers for your situation is a face-to-face consultation with our physician.