What is Endometriosis?
Endometriosis is a benign condition in which the tissue that forms the lining of the uterus (called endometrium) grows in places outside the uterus. The disease is associated with pelvic pain and infertility.
How Common is Endometriosis?
Because surgery is the only reliable method to diagnose endometriosis and generally is not performed on women with no symptoms, exactly how common the disease is remains unknown.
- 1-7% of women seeking elective sterilization are found to have endometriosis with no symptoms.
- 12-32% of women of reproductive age and pelvic pain are found to have endometriosis.
- 9-50% of women with infertility are found to have endometriosis, and
- 50% of teens with chronic pain or painful period are found to have endometriosis.
The overall prevalence of endometriosis in reproductive age women is estimated to be somewhere between 3% to 10%.
Who is at Risk to Have Endometriosis?
Women with certain forms of congenital uterine abnormality which obstruct normal outflow of menstrual bleeding are at risk to have endometriosis. Early onset of first mense and frequent menstrual cycles have been associated with increased risk for endometriosis. Endometriosis occurs more often in women who have never had children. Pregnancy has a protective effect. Women with a mother, sister, or daughter who have had endometriosis are more likely to have it.
What Causes Endometriosis?
The exact cause of endometriosis is not fully understood. There are several theories on the origin of endometriosis but no one particular theory explains all cases of endometriosis.
- Sampson’s theory or retrograde menstrual flow
- Some of the menstrual tissue that shed during menstruation flow backward through the fallopian tubes into the pelvic cavity where they settle down on the surfaces of pelvic organs and become endometriosis.
- Coelomic (the lining of the chest, abdominal, and pelvic cavity) metaplasia (change in cell type)
- The lining of the pelvic cavity, abdominal cavity and the chest cavity spontaneously (after exposed to certain unknown stimuli) transforms into tissue that resembles the uterine lining (endometrium).
- Spreading of the endometrial cells via the blood stream or lymphatic system
- Altered immune response in women with endometriosis
- 75-90% of women are found to have menstrual blood in the pelvis during elective laparoscopy performed at the time of mense and yet most women do not develop endometriosis. The altered immune response in women with endometriosis, and supported by recent research data, explains how endometriosis develops in some but not all women.
Where are the most common places in the body where endometriosis is found?
Endometriosis is most often found in places within the pelvis:
- Ovaries: endometriosis can be found as a spot or two on the surface of the ovary, or the endometriosis can be completely enclosed in a cyst (called endometrioma)
- Fallopian tubes
- Surface of the uterus
- Cul-de-sac: the space behind the uterus at the bottom of the pelvis
- Bowel and rectum
- Bladder and ureters
- Peritoneum: the lining of the pelvic and abdominal wall.
What are the Symptoms of Endometriosis?
Pelvic Pain
Pelvic pain is the most common symptom associated with endometriosis. Pain may occur with sex, during bowel movements or urination, or before or during menstrual cycle. The amount of pain does not always tell how severe the condition is. Many women with endometriosis have no pain symptoms, only to find out they have endometriosis when they have difficulty to get pregnant.
Infertility
See Does endometriosis cause infertility?
How does Endometriosis Lead to Pelvic Pain?
There are several ways endometriosis cause pain.
Endometriosis responds to changes in hormones. It breaks down and bleeds like the lining in the uterus (endometrium) during the menstrual cycle. The localized bleeding of endometriosis lesions in the pelvis, combined with the inflammatory chemicals released by specialized white blood cells in the pelvis lead to pelvic pain.
As a result of the inflammatory reactions, adhesions (scar tissue that binds together the surfaces of tissues) form. Adhesions can cause pain either as a direct pulling or compression effect or indirectly via its effect on the nerve endings that give pain perception in the pelvic and abdominal cavities.
When endometriosis infiltrates into the upper vaginal wall, rectal wall or other tissue in the deepest part of the pelvic cavity, it irritates the nerve endings in the region, causing pain with sex, bowel movement or chronic pelvic pain.
Does Endometriosis Cause Infertility?
Endometriosis is strongly associated with infertility, up to 30% to 50% of infertile women have the disease, and often at a more severe stage than fertile women. Numerous research data support the conclusion that endometriosis decrease fertility.
How does endometriosis cause infertility?
Two major theories have been proposed to explain how endometriosis leads to infertility.
- Abnormal anatomic relationship between the tube and the ovary – When endometriosis is advanced to a moderate to severe stage, the ovary is typically wrapped around or bound by adhesions. Likewise, the neighboring fallopian tube is often twisted or blocked. When the anatomy is so distorted, the egg can no longer be picked up easily by the fallopian tube.
- Excessive production of inflammatory chemicals – Specialized white blood cells in the pelvis are shown to produce a number of inflammatory chemicals designed to curb the growth of endometriosis. Unfortunately, these chemicals create a “hostile” environment in the pelvis. Research has shown that these inflammatory chemicals impair normal function of the ovary, tube, or the uterine lining, as well as the survival of sperm, egg and embryos.
Does endometriosis cause increased miscarriage?
Some older studies have observed an increased risk for early pregnancy loss in women with endometriosis. However, in more recent studies, miscarriage rates in untreated women with endometriosis are found to be no different.
How is Endometriosis Diagnosed?
Clinical symptoms
Classic symptoms of endometriosis are progressively worsening of painful period, pain with sex, and cyclic bowel or bladder symptoms. However, the severity of endometriosis does not correlate with the severity of disease. Women with advanced disease may have few or no symptoms, whereas those with minimal or mild disease may have debilitating pain.
Pelvic examination
A pelvic examination is a physical examination of a woman’s reproductive organs. Findings at pelvic examination vary widely, depending on the location and the extent of the disease. Sometimes red or blue colored implants may be seen on the cervix or in the upper portion of the vaginal wall. Uterus is often “tilted” backward and relatively fixed in position. Pain or an enlarged ovary may be found in women with endometriosis on the ovary. Deeply infiltrating endometriosis in the upper vaginal wall or the rectum may also be found on pelvic examination.
Ultrasound
Ultrasound is best suited to detect an ovarian endometriosis cyst (endometrioma) but cannot identify pelvic adhesions or superficial endometriosis growths in the pelvis.
Magnetic resonance imaging (MRI)
MRI does not use ionizing radiation like X-rays or computed tomography (CT). An MRI scanner uses a combination of electromagnetic field and radio frequency to allow a construction of an image of the scanned area of the body. On some occasions when rectal or vaginal nodule is found, an MRI of the pelvis may be performed to help differentiate deeply infiltrating pelvic endometriosis from other diseases. Like ultrasound, MRI may be helpful to tell the difference between an ovarian endometrioma from other ovarian masses, but has limited value to diagnose superficial endometriosis growth.
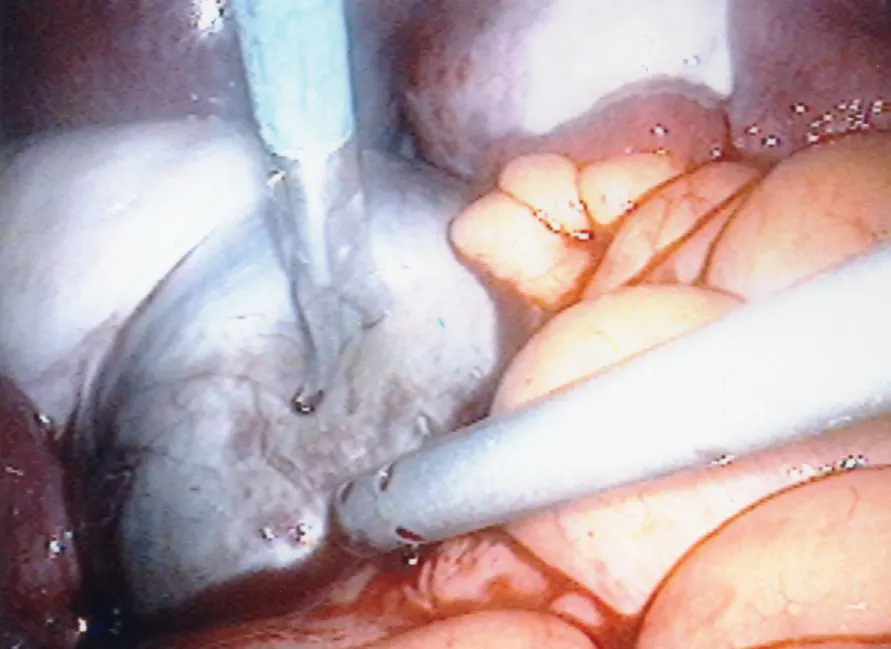
Laparoscopy
Laparoscopy is the gold standard for the diagnosis of endometriosis. Laparoscopy is called “minimally invasive” surgery because the surgeon makes very small incisions at (or around) the belly button and the lower portion of the belly. Compared with laparotomy (the traditional technique for surgery where the abdomen is incised and opened) laparoscopy offers the advantages of better visibility, less tissue trauma, smaller incisions, and a speedier recovery from surgery.
During laparoscopy, a thin (5mm of less in diameter) light-transmitting instrument is inserted into one incision. The laparoscope is connected to a camera which can project live images of the pelvic organs on a TV monitor. Sometimes a small amount of tissue is removed (called a biopsy) at the time of laparoscopy and sent to a lab to be further studied.
What are the Treatments for Endometriosis?
Medical treatment
Medical treatment for endometriosis have been based on Sampson’s theory of retrograde menstruation and implantation. The objectives of treatment have been to reduce or eliminate cyclic menstruation, thereby decreasing the amount of menstrual tissue and the likelihood of new lesions will develop. At the same time, it is assumed that by suppressing the normal uterine lining (the endometrium), the same suppression will happen with existing endometriosis lesions.
Medical treatment for pain
Medical treatment is often used to reduce the menstrual flow and menstrual pain. Sometimes medical treatment may be recommended before resorting to surgical treatment unless there is evidence to suggest an acute process. There is no evidence that one medical treatment is more superior than other. They have similar effectiveness in pain relief and recurrence rates.
Medical treatment for infertility
Medical treatment does not improve pregnancy rate in women with endometriosis and infertility, in part because ovulation is suppressed with medical treatment. In older women with more limited time to conceive, medical therapies may adversely affect their chance of pregnancy by delaying conception. Generally medical treatment is not effective for endometriosis cyst on the ovary (endometrioma) or pelvic adhesions.
Hormonal birth control
Any one of the hormonal methods of birth control reduces menstrual bleeding and menstrual pain. These include birth control pill, skin patch, vaginal ring, shot, hormonal IUD and implant. Up to 75-90% of women with pain associated with endometriosis can experience effective relief when combination of birth control pill is taken continuously.
Non-steroidal anti-inflammatory medication (NSAIDs)
Gonadotropin releasing hormone agonist (GnRH agonist)
GnRH agonists (e.g. leuprolide, nafarelin, buserelin) work by “turning off” the ovaries, causing a temporary and reversible menopause. They are given as an injection, an implant, or nasal spray. They are very effective in relieving pain in women with endometriosis. Side effects include hot flashes, mood swing, irritability, joint pain and muscle ache. They cannot be used for longer than six months consecutively due to risk of bone loss (osteoporosis). In an effort to prevent the bone loss problem with GnRH agonist, combined estrogen-progestin add-back regimens have been studied. Numerous clinical trials have shown that hormone add-back regimens protect bone and reduce symptoms of hot flashes without sacrificing control of pain associated with endometriosis.
GnRH agonists are sometimes used to decrease the size of endometriomas, but not to eliminate them. Generally endometrioma larger than 1cm does not respond well to GnRH agonist or other medical treatment.
Aromatase inhibitors
Although not approved by the Food and Drug Administration (F.D.A.) for the treatment of endometriosis, aromatase inhibitors (anastrozole 1mg daily, letrozole 2.5mg daily) have been found in several small studies to be effective for the treatment of pain associated with endometriosis. Aromatase inhibitors suppress estrogen production by blocking the last biochemical step where testosterone (a male sex hormone) is converted to estrogen ( a female sex hormone).
Side effects of aromatase inhibitors include bone loss and hot flashes. They can also stimulate multiple ovarian cysts, thereby making it necessary to be used in combination with a GnRH agonist or synthetic progesterone (e.g. norethindrone acetate 5mg daily) to avoid the complication.
Surgical treatment
While the objectives of medical treatment for endometriosis are to reduce or eliminate cyclic menstruation, objectives of surgical treatment for endometriosis are
to eradicate all visible endometriosis lesions,
to remove pelvic adhesions, and
to restore normal anatomical relationships.
Surgical treatment for pain
Surgical treatment of pain associated with endometriosis is reported in one study to give pain relief in about two-thirds of women six months after surgery. Other trials have reported success in pain relief anywhere from 70-100% of women with endometriosis. As in medical treatment of pain associated with endometriosis, recurrent disease and pain after conservative treatment with surgical removal of endometriosis are common. About 10-20% per year for women treated with surgery is expected to have recurrence of pain. Pain recurrence is in part due to recurrence of endometriosis lesions in the same or neighboring areas of the pelvis.
Deeply infiltrating endometriosis in the vagina or rectum requires extensive surgery with thorough dissection. Often a portion of the upper vagina may be removed along with a short segment of the rectum but excellent pain relief can be achieved.
Surgical treatment for infertility
The effectiveness of surgical treatment of infertility depends on the amount and extent of the disease. A multi-center Canadian trial found that surgical treatment (removing the lesions) of mild endometriosis among women with infertility was twice as effective (to become pregnant) as in untreated women. In another smaller Italian trial, no difference between surgical treatment or no treatment was found. When the data from these two studies are combined, a smaller (about 60%) improvement in infertility is found.
No study has been done to compare surgical treatment versus no treatment among women with moderate to severe endometriosis and infertility. Small studies have reported successful pregnancy anywhere from 30% to 50% within 1-3 years after surgical treatment of moderate to severe endometriosis.
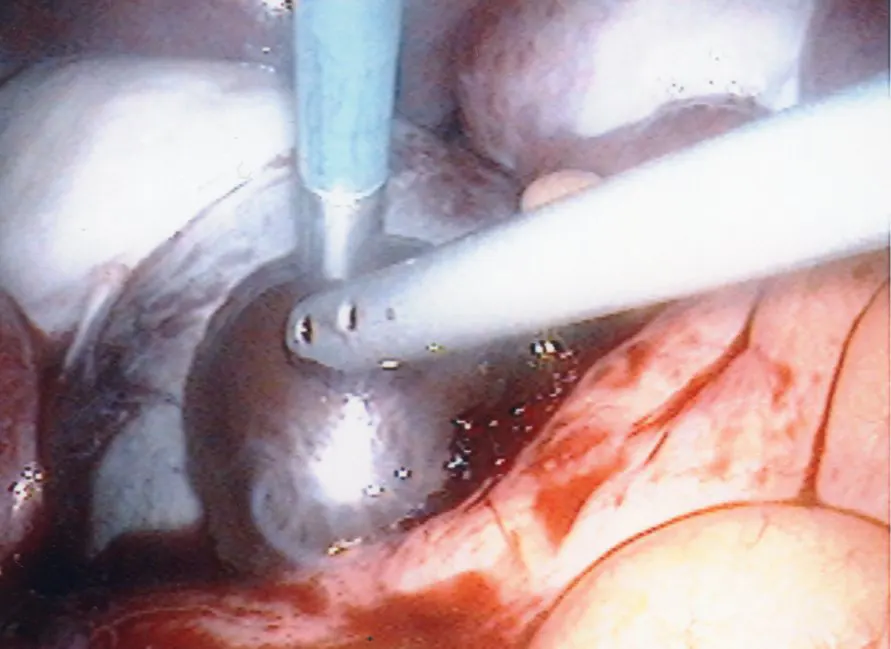
Surgical treatment of endometrioma
Ovarian endometriosis cysts (endometriomas) bigger than 1cm generally do not respond to medical treatment. The wall of the endometrioma must be removed (peeled from the adjacent normal ovarian tissue) in order to minimize recurrence of cyst and pain, and to maximize fertility among women who were infertile. Surgical removal of endometrioma can sometimes lead to compromised ovarian function. Excessive ovarian tissue may be removed at the time of surgery or the blood flow to the ovary may be compromised. Because of this potential risk, it is generally recommended to remove endometrioma only if it is symptomatic (painful) or large (bigger than 3cm).
Laparoscopic treatment of endometriosis
Except in rare cases where laparoscopy is contra-indicated, laparoscopy (as opposed to the traditional surgery with laparotomy) is the surgical method of choice in the treatment of endometriosis. Laparoscopy offers a proper diagnosis of endometriosis, giving definitive information on the amount, location and depth of endometriosis (staging of the disease). It also offers an opportunity for the surgeon to treat the diseases at the same operation. Additional surgical steps can be taken to restore the pelvis to normal. The endometriosis lesions may be eradicated with a number of methods (laser, electrical cauterization or simple cutting away the lesions). Adhesions may be removed to free up the ovary and the tube. Sometimes the occluded tube(s) may be repaired.
Hysterectomy
Hysterectomy is the removal of the uterus. The ovaries may or may not be removed. Endometriosis is less likely to come back if the ovaries also are removed. Hysterectomy is a last resort when medical treatment and conservative surgery have not worked, extensive disease, and a woman no longer wishes to have any children. Unfortunately, in spite of hysterectomy and removal of the ovaries, there is a small chance that pain symptoms will come back.
Combined medical and surgical treatment
For a woman with primarily pelvic pain associated with endometriosis and fertility is not her immediate concern, post-op medical treatment (continuous or cyclic hormonal birth controls) may be appropriate especially in women with extensive disease or significant residual disease that could not be completely removed at the time of surgery.
Because the highest pregnancy rates after conservative surgery in infertile women with endometriosis are observed in the first year after operation, medical treatment (which suppresses ovulation) after surgery will eliminate that benefit. Generally young woman with limited disease and has no additional reason for her infertility can be given a short duration (usually for 6-9 mos) to attempt to conceive on her own after surgical treatment.
For older women, women with longer durations of infertility, or advanced degree of endometriosis, an aggressive treatment approach (after surgical treatment) to actively pursue pregnancy (controlled ovarian stimulation and intrauterine insemination or in-vitro fertilization) is recommended.
What Treatment is Right for Me?
Treatment for endometriosis depends on whether you want to have children, severity of your symptoms, findings on physical examination and/or ultrasound examination of the pelvis, extent of the disease and whether medical or surgical treatments have been attempted in the past.
Medical treatment with NSAID and/or hormonal birth control for painful period or other endometriosis related pain symptoms is appropriate before considering surgical treatment, especially among adolescents. On the other hand, women with suspected ovarian endometriosis cyst (endometriomas) or more advanced disease are better treated surgically.
If you have infertility and endometriosis of a mild to moderate nature, surgical treatment with a laparoscopy along with removal of endometriosis lesions, freeing up the adhesions and restoring the normal anatomy of the fallopian tubes and ovaries can increase your chances of becoming pregnant naturally, especially if you have good ovarian reserve. Surgery to remove large (greater than 3cm in diameter) endometriosis cyst on the ovary may also improve fertility rates. There is a limit as to how much surgery can improve pregnancy rates. With long standing infertility and advanced disease where there are extensive endometriosis lesions, severe scarring (adhesions), and/or the ovaries are completely immobilized and the tubes are destroyed beyond repair, treatment with hormonal birth controls for 6-8 weeks followed immediately by in-vitro fertilization is more appropriate and effective.
Schedule a Consultation
Contact Us
If you are experiencing a medical emergency, call 911 or go to the nearest emergency room.
We understand you may have a lot of questions. Additionally, each couple or individual has a unique set of circumstances. To this end, the best way to get answers for your situation is a face-to-face consultation with our physician.
Schedule a Consultation
Contact Us
If you are experiencing a medical emergency, call 911 or go to the nearest emergency room.
We understand you may have a lot of questions. Additionally, each couple or individual has a unique set of circumstances. To this end, the best way to get answers for your situation is a face-to-face consultation with our physician.