When to Test for Infertility
Almost 90% of couples conceive after a year of unprotected intercourse. Evaluation of infertility is indicated if the female partner is under 35 years of age and the couple has been trying to conceive for one year. Immediate evaluation and treatment of infertility is appropriate in cases of known problems that impact fertility such as irregular menstrual cycles, pelvic endometriosis, past history of pelvic infection or sexually transmitted disease, previous abdominal or pelvic surgery, or severe male factor infertility.
Because fertility declines with advancing age of the female, evaluation of infertility is warranted for a couple when the female partner is older than 35 and has been trying to conceive for 6 months without success. In the subgroup of women older than 40 years of age, a more aggressive approach in evaluating and treating infertility is generally recommended because of the high likelihood for significant and rapid loss of ovarian reserve in this age group.
Infertility Evaluation
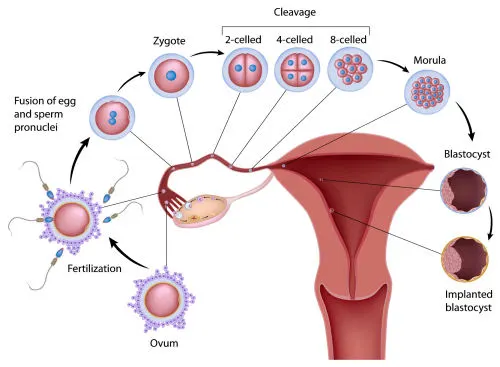
The efficiency and accuracy of the infertility evaluation is a key factor in developing the appropriate treatment plan to achieve the couple’s ultimate goal–a healthy baby. The basic elements of an infertility evaluation target ovarian function, tubal and uterine anatomy, and ability of the sperm to reach the fallopian tube and fertilize an egg or male factor.
Infertility Diagnostic Testing
After a thorough history and physical examination, additional infertility diagnostic testing is undertaken to refine the diagnosis. These initial tests are:
- Ovarian reserve testing (one or more of the following tests may be taken)
- Day 3 blood test for FSH (follicle stimulating hormone) and estradiol (estrogen)
- Day 3 antral follicle count: an ultrasound examination to measure the number of follicles between 4-8 mm on both ovaries.
- Blood test for anti-mullerian hormone
- Clomiphene citrate challenge test
- Testing for tubal and/or uterine anatomy
- Hysterosalpingogram (tubal dye test) and/or
- Sonohysterogram (an ultrasound examination)
- Testing to determine ovulation
- Ultrasound to document the time of ovulation
- Blood test to check progesterone level in mid-luteal phase
- Testing to assess mucus and sperm interaction
- Post coital test: to see if cervical mucus is optimal and sperm survival is sufficient
- Semen testing
- Semen analysis
- Anti-sperm antibodies
In the majority of cases this list of information is enough to indicate the appropriate initial treatment plan. Laparoscopy is not routinely indicated because it has the risks of surgery and does not usually change the initial treatment plan. However, laparoscopy may be indicated if there is suspected endometriosis or tubal disease based on the history, physical findings or ultrasounds examinations; or if there are other specific gynecologic reasons to perform this procedure.
Basic Workup
With the following basic work up, which can be completed within one menstrual cycle, a couple can be efficiently evaluated, specific major causes of infertility identified, and treatment options considered. As with all medical testing, an infertility evaluation must be tailored to each patient’s situation.
Day 3 FSH and Estradiol, Antral Follicle Count and Anti-Mullerian Hormone
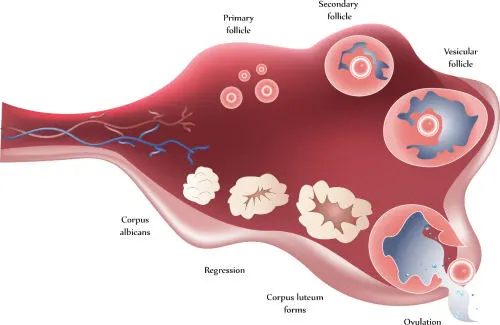
Ovarian reserve testing is an attempt to estimate the size and quality of the remaining ovarian follicular pool. Ovarian reserve essentially estimates the likelihood of success with treatment using the patient’s own eggs. Ovarian reserve tests include both blood tests and ultrasound examination of the ovaries.
Diminished ovarian reserve may be suspected by elevation in either the FSH or the estradiol. The FSH levels will vary somewhat by the endocrine lab and the assay used. Unfortunately the prognosis is based on the highest, but not necessarily the most recent, FSH level. It is advisable to obtain an opinion and possible further testing from an infertility specialist for those patients with abnormal levels, especially those under age 35.
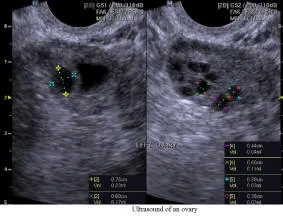
An antral (early) follicle count can be used to further clarify the patient’s ovarian reserve. This is done on or about the third day of the cycle with an ultrasound examination. Antral follicle count is the sum total of all follicles in both ovaries that are 4-8 mm in average diameter.
Recently, anti-Mullerian hormone (AMH) is advocated as an additional marker for ovarian reserve. Unlike FSH level, AMH level does not fluctuate with the menstrual cycle or affected by medications such as birth control pill.
For more information on Ovarian Reserve, Age and Fertility:
Ovarian reserve (predicting fertility potential in women)
Does My Age Affect My Fertility
Reproductive aging in women
Age and Fertility
Hysterosalpingogram & Sonohysterogram
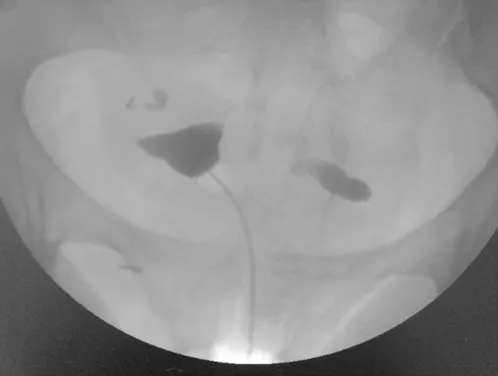
The hysterosalpingogram (HSG) is still the best, and least invasive method of evaluating the inside of uterine cavity and patency of the fallopian tubes. In addition, a sonohysterogram (ultrasound after saline is placed in the uterus through a catheter) is a relatively non-invasive way of evaluating the uterine cavity alone if intrauterine pathology is suspected.
Both tests can uncover uterine abnormalities such as adhesions or polyps inside the uterus, or fibroid that protrudes or distort the uterine cavity. But, only the HSG can evaluate tubal abnormalities such as blockage or occlusion. A hydrosalpinge is a blocked fallopian tube distended by fluid within. Abnormalities on an HSG or sonohysterogram may warrant further evaluation with laparoscopy and or hysteroscopy.
Top: Normal HSG; Bottom: HSG showing blockage of both tubes
Ultrasound Examination of the Pelvis
Ultrasound examination of the pelvis is a safe, painless and indispensible part of an infertility diagnostic testing. Ultrasound examination of the ovaries for antral follicle count is one of many methods of ovarian reserve testing. Ultrasound is very reliable to identify uterine anatomy and abnormality within the uterine cavity as in sonohysterogram. Ultrasound examination of ovarian follicle, which contains the egg within, for its proper development and the timing of its release is critical to the evaluation of infertility.
Left to Right: Ultrasound of Uterus, Ultrasound of Ovary, Ultrasound of a 7 Week Pregnancy
Post Coital Test
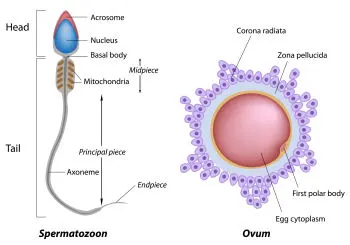
The post coital test or PCT is an examination of the interaction between sperm and cervical mucus. Once the timing of ovulation is determined accurately, the next step is to assess if the sperm can survive in the cervical mucus. A couple is instructed to have intercourse the day of ovulation. The female partner is examined in the next morning. A sample of the cervical mucus is observed under the microscope to see if adequate sperm survives in the mucus. Poor cervical mucus may be suggestive of incorrect timing, cervical inflammation or intrinsic poor cervical mucus production as in previous cervical surgery. If cervical mucus is clear and abundant but no or few live sperm is found, it may be a problem of sperm longevity, low sperm number, poor sperm motility or an immune reaction against the sperm.
Mid-luteal Phase Progesterone
Menstrual cycle regularity and premenstrual symptoms are reliable medical history indicating the probability of ovulation. However, some women ovulate but fail to produce adequate quantities of progesterone (luteal phase deficiency) following ovulation. The clinical tests for ovulation (e.g. temperature chart, positive ovulation predictor kit) are not sufficient to diagnose luteal phase deficiency. We recommend obtaining a progesterone level approximately 8 days after detection of the LH surge.
Semen Analysis
It is important to perform this test early in the infertility evaluation since in at least 40% of couples experiencing infertility the sperm quality will be a factor. The test will identify a potential male factor by checking the semen volume, sperm concentration, motility and morphology (sperm size and shape) in a semen sample. Bear in mind however semen analysis is not a perfect test. There are males with “poor” semen analysis and sire children with no difficulty. Conversely many males with normal semen analysis but have low fertilization in an IVF cycle.
Click here to view microscopic examination of sperm.
References
- Optimizing Natural Fertility
- Evaluation of the Uterus
- Ovulation Detection
- Infertility: An Overview
- Diagnostic Testing for Male Factor Infertility
- Diagnostic Testing for Female Infertility
- Age and Fertility
- Ovarian reserve (predicting fertility potential in women)
- Does My Age Affect My Fertility
- Reproductive Aging in Women
- Hysterosalpinogram (HSG)
- HSG Radiology Information
- Sonohysterogram (SHG)
- Infertility and Men
- Infertility and Women
References on Male Fertility
Schedule a Consultation
Contact Us
If you are experiencing a medical emergency, call 911 or go to the nearest emergency room.
We understand you may have a lot of questions. Additionally, each couple or individual has a unique set of circumstances. To this end, the best way to get answers for your situation is a face-to-face consultation with our physician.
Schedule a Consultation
Contact Us
If you are experiencing a medical emergency, call 911 or go to the nearest emergency room.
We understand you may have a lot of questions. Additionally, each couple or individual has a unique set of circumstances. To this end, the best way to get answers for your situation is a face-to-face consultation with our physician.